Key Takeaways
- Veterans face unique challenges that increase their risk of addiction.
- PTSD and traumatic brain injuries are closely linked to substance abuse.
- Tailored treatment programs are critical for recovery success.
Introduction to Statistics on Substance Abuse & Alcohol Abuse Among Veterans
Transitioning from military service to civilian life can be overwhelming for many Veterans. The effects of trauma, stress, and physical injuries often lead to substance use as a coping mechanism. Addiction among Veterans is a growing concern, with many struggling in silence due to stigma and a lack of resources.
This article sheds light on addiction statistics for Veterans, the underlying factors, and how specialized programs can support their recovery journey.
The Prevalence of Drug Use and Addiction Among Veterans & Military Personnel
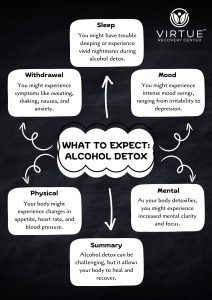
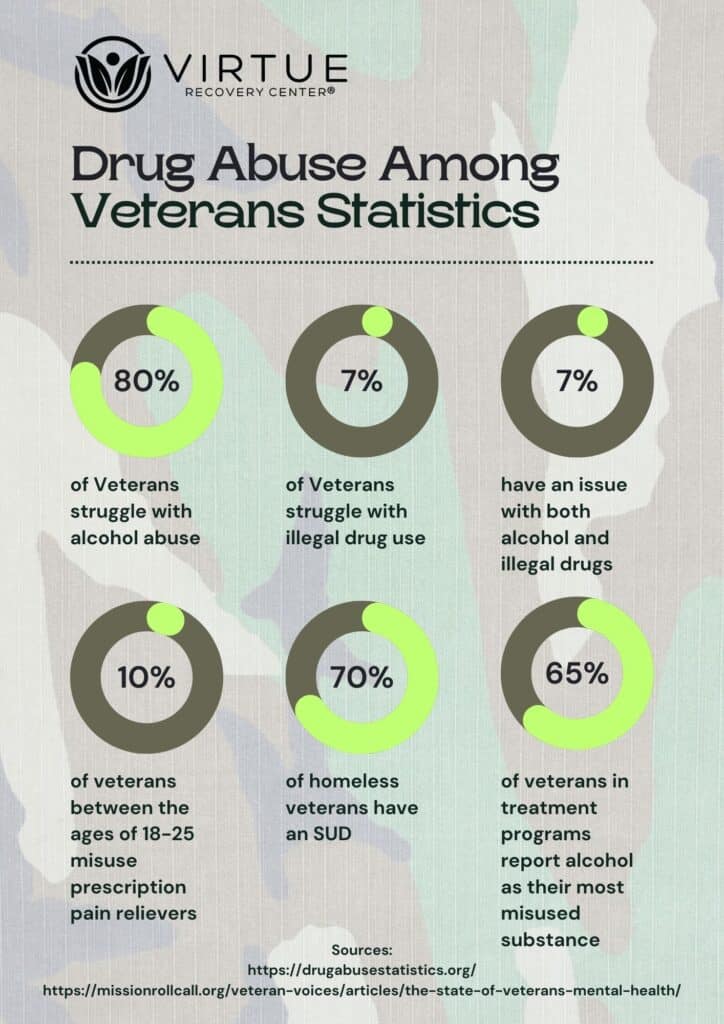
Addiction is a significant issue in the veteran community, with substance use disorders (SUDs) affecting many who have served. Alcohol misuse is particularly common, but other substances, including prescription medications and illicit drugs, also pose challenges.
Veterans are five times more likely to develop alcohol use disorders compared to civilians. Many use alcohol to manage stress, anxiety, or physical pain caused by their service. Additionally, younger Veterans frequently misuse prescription pain relievers, which often leads to dependence or even addiction.
Despite the high prevalence of addiction, less than 12% of Veterans with SUDs receive the professional treatment they need. Barriers such as stigma, limited access to care, and under-enrollment in VA healthcare contribute to this treatment gap.
Connection Between PTSD and Substance Abuse Among Veterans
Post-traumatic stress disorder (PTSD) is a common diagnosis among Veterans, especially those who served in combat zones. The condition is characterized by flashbacks, heightened anxiety, and emotional numbness, all of which significantly impact daily life.
Many Veterans turn to drugs or alcohol to cope with these overwhelming symptoms. Unfortunately, this self-medicating behavior often leads to addiction. Veterans with PTSD are three to four times more likely to develop SUDs than those without the condition. Co-occurring mental health disorders, such as depression, further complicate recovery efforts.
The combination of PTSD and addiction is a cycle that requires specialized care. Effective treatment programs address both conditions simultaneously, ensuring a holistic approach to recovery.
The Role of Traumatic Brain Injuries in Addiction
Traumatic brain injuries (TBIs) are another factor contributing to addiction among Veterans. These injuries, often caused by explosions or physical trauma during service, can lead to long-term cognitive and emotional difficulties.
Veterans with TBIs may struggle with memory loss, impulsive behavior, and difficulty regulating emotions. These challenges often make them more susceptible to substance use as a means of coping. Over 400,000 U.S. service members have reported TBIs since 2000, highlighting the scale of this issue.
Addiction treatment for Veterans with TBIs must be tailored to address their unique needs, focusing on both physical and mental health recovery.
Homelessness and Its Impact on Veterans and Addiction
Veterans experiencing homelessness often face significant barriers to accessing addiction treatment. Lack of stable housing, healthcare, and social support exacerbates substance use problems, creating a vicious cycle that is difficult to break.
Homeless Veterans make up 11% of the homeless adult population in the U.S. Among those in substance use treatment, one in five is without stable housing. Addressing homelessness as part of addiction recovery involves connecting Veterans to resources like transitional housing and community support programs.
Specialized Treatment for Veterans Suffering From Substance Use Disorder
Effective addiction treatment for Veterans goes beyond addressing substance use. It incorporates therapies for PTSD, TBIs, and other co-occurring conditions to ensure comprehensive care.
Dual diagnosis programs are essential, as they simultaneously treat mental health issues and addiction. Holistic therapies promote overall well-being, such as mindfulness, physical fitness, and art therapy.
Legislation like the Hannon Act has expanded access to mental health services, including alternative therapies like yoga and acupuncture. These resources provide Veterans with new pathways to healing and recovery.
Conclusion
Veterans face unique challenges that put them at a higher risk of addiction. PTSD, TBIs, and homelessness contribute to the widespread prevalence of substance use disorders in this community. However, hope exists through specialized treatment programs designed to address these interconnected issues.
If you or a loved one is a veteran struggling with addiction, call Virtue Recovery Las Vegas at 866-520-2861. Our compassionate team is here to guide you toward a healthier, sober future.
FAQs About Statistics For Veterans and Addiction
Why do Veterans experience higher rates of addiction?
Veterans often face challenges such as PTSD, traumatic brain injuries, and the stress of transitioning to civilian life, which increase their risk of addiction.
What substances are most commonly misused by Veterans?
Alcohol is the most frequently misused substance among Veterans, followed by prescription medications and marijuana.
How can PTSD contribute to substance abuse?
PTSD symptoms like anxiety and flashbacks often lead Veterans to self-medicate with drugs or alcohol, increasing their likelihood of addiction.
What treatment options are available for Veterans with addiction?
Treatment options include dual diagnosis programs, inpatient and outpatient care, and holistic therapies tailored to Veterans’ unique needs.
How can I support a veteran struggling with addiction?
Encourage them to seek professional help, listen without judgment, and connect them with specialized resources like Virtue Recovery Las Vegas.
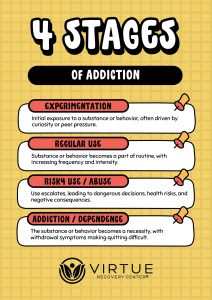
What is the most common cause of addictive behavior?
The most common cause of addictive behavior is a combination of genetic predisposition, environmental factors, and mental health conditions such as stress or trauma. These elements can alter brain chemistry, making individuals more vulnerable to developing compulsive habits or dependency on substances.
Resources
https://missionrollcall.org/veteran-voices/articles/the-state-of-veterans-mental-health/
https://nida.nih.gov/publications/drugfacts/substance-use-military-life